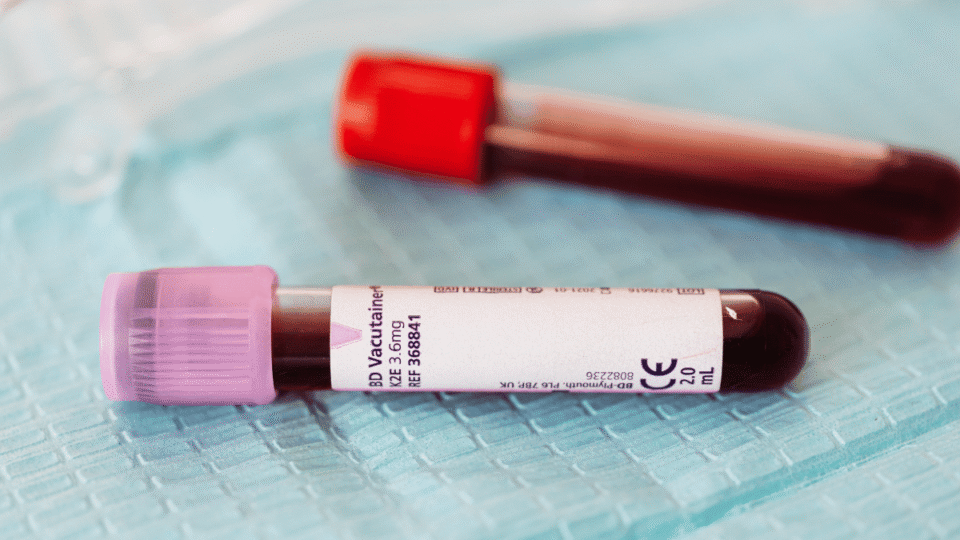
Because severe injuries frequently lead to massive bleeding, clinicians are required to act quickly to restore lost blood and stabilize the patient. To accomplish this objective, massive transfusion programs were created. These programs deliver big quantities of blood products, typically ten or more units of red blood cells (RBCs), within the initial day of treatment.
For several years, medical organizations recommended using RBCs first, then plasma and platelets secondarily if necessary. However, physicians who specialize in treating traumatic injuries noticed a disturbing pattern. Many patients died early due to uncontrolled bleeding before they were able to get sufficient amounts of plasma and platelets to treat their coagulation difficulties.
This pattern led to a major query among healthcare professionals specializing in trauma treatment. Can altering the ratios of plasma and platelets to red blood cells enhance survival for the most seriously injured patients?
John B. Holcomb and a group of leading trauma specialists, including Dr. Martin A. Schreiber, released a landmark study in 2008 that would contribute to modern medicine’s evolving thoughts on blood transfusion techniques in trauma environments. The title of their study, “Increased plasma and platelet to red blood cell ratios improve outcome in 466 massively transfused civilian trauma patients,” examined the effects of various transfusion ratios on patient survival.
The researchers studied the data of 466 civilian trauma patients who had to undergo massive transfusions. Each patient studied was treated at one of the major trauma centers. The researchers measured the amount of plasma and platelets each patient received relative to the amount of red blood cells each received. Afterward, the researchers compared the outcomes for each patient during the first 24 hours and during their entire hospital stay.
Prior to this study, most hospitals followed a 1:3 plasma-to-RBC ratio, i.e., one unit of plasma per three units of red blood cells. Platelet guidelines were even less consistent. Many patients received platelets only after laboratory tests showed decreased clotting ability. Other patients received platelets only after major bleeding was apparent.
Dr. Holcomb and his colleagues analyzed the effect of altering these ratios. When patients received early, high amounts of plasma and platelets and were administered these in a ratio closer to 1:1 with red blood cells, the survival rate improved dramatically. The benefit was especially pronounced during the first six hours following the injury. That time frame is when hemorrhagic death, or death resulting from uncontrolled bleeding, is most common.
The explanation for the improvements in survival rates is related to the body’s response to severe traumatic injury. The body’s clotting mechanisms and platelet counts are disrupted by the loss of large amounts of blood. If there is no immediate correction to these deficiencies, the body loses the capacity to stop the bleeding process, regardless of how well the surgeon attempts to repair the damage. Red blood cells add to the volume of blood, however they do not offer the coagulating properties that are provided by plasma. Plasma contains proteins essential for clot formation. Platelets assist in sealing damaged blood vessels and providing a stable clot.
When the three components are administered together, rather than waiting until bleeding worsens, this helps prevent a serious clinical condition known as the lethal triad. This condition includes hypothermia, acidosis, and coagulopathy. Once the lethal triad develops, survival rates decline rapidly.
The results of this study of nearly five hundred patients validated what military physicians had already observed in combat care. Balanced transfusion ratios produce better survival rates. The researchers found that higher plasma-to-platelet ratios decreased early mortality and improved survival rates throughout the remainder of the hospital stay. The researchers also found that the majority of patients who survived the critical first few hours experienced better long-term recovery.
One of the most significant points emphasized in the study is that timing is crucial. The researchers did not simply analyze which blood components were administered; they also analyzed when they were administered. The earlier administration of plasma and platelets resulted in better outcomes than late administration. Trauma teams that utilized ratio-based protocols, rather than reactive transfusions based solely on lab test results, were able to stabilize patients faster.
The findings of this study greatly influenced the development of what is now commonly referred to as damage-control resuscitation. Prior to this study, trauma teams relied on large volumes of normal saline to treat shock, or initially administered only red blood cells. Trauma teams began using balanced blood product resuscitation immediately upon initiating massive transfusions.
This study also contributed to a change in how blood banks and hospitals prepare for massive transfusions. Trauma centers began developing massive transfusion protocols that enabled rapid delivery of pre-determined blood product packages. Emergency teams were able to access red blood cells, plasma, and platelets in the appropriate ratios instantly, rather than having to order each item individually. The study helped reduce delays that previously affected treatment success.
Additionally, the study stimulated further discussion of the role of platelets in early trauma treatment. Platelets are generally more difficult to store and transport than the other blood products. The study demonstrated a clear survival advantage to platelet use, encouraging hospitals to update their procedures for storing and transporting platelets.
The study’s impact on shaping trauma practices today is still felt. Many current recommendations worldwide recommend a 1:1:1 ratio of red blood cells, plasma, and platelets for the management of massive bleeding. Both military and civilian trauma systems have adopted these principles.
In addition to demonstrating scientifically valid findings, the study also emphasizes the value of collaborative research efforts in trauma treatment. The list of authors includes leading figures in surgery, critical care, blood banking, and emergency response. Dr. Martin A. Schreiber, one of the co-authors of the study, has long been recognized for his contributions to the advancement of trauma resuscitation and the improvement of outcomes for patients who suffer traumatic injuries. The combined efforts of these researchers continue to influence education programs for physicians, surgeons, and first responders.
A key factor in the study’s positive impact was the size of the patient population. Previous studies examining the topic had smaller patient populations, making the reliability of their conclusions difficult to establish. Due to the larger patient population studied (n=466), the conclusions were more robust and demonstrated a clear trend. Balanced transfusion not only makes theoretical sense, it changes what occurs in emergency departments.
The study established a connection between military and civilian trauma practices. Military teams treating combat casualties identified the potential for high ratio early transfusions to result in improved survival rates. When the civilian medical community adopted similar practices following confirmation of the survival advantage demonstrated in studies of civilian patients, the widespread adoption of these life-saving techniques accelerated.
Trauma is one of the leading causes of death globally, particularly among young adults. Despite advances in medical technologies, the primary cause of potentially preventable trauma-related deaths remains early bleeding. By identifying a method for managing critical trauma cases, the study helped address this issue.
Progress in science often occurs incrementally. The publication of this study represents one of those significant incremental steps. The study helped alter the approaches used by clinicians to manage massive transfusions and continues to serve as a reference point for trauma care nearly two decades later. The study demonstrates clearly. Timely and balanced transfusions can provide a valuable resource for trauma teams to reduce early mortality and support better long-term recovery.
The study influenced not only the clinical practices of trauma teams but also the preparation of blood banks and trauma centers for massive transfusions.
If your colleague, friend, or family member is making an impact in their career, industry, or community, we want to hear about it.